“What is my cholesterol?”
“Do I have high cholesterol?”
“Should I be taking a cholesterol pill?”
These are all common and important questions. These questions arise every day in family medicine. The topic of cholesterol is fascinating and evolving. In recent years, research has shown exciting new ways to address cholesterol with patients.
WHY IS CHOLESTEROL IMPORTANT?
Over time, plaques and blockages can form in our blood vessels. This is a process known as “atherosclerosis.” Many factors can make atherosclerosis worse, such as smoking, high blood pressure, and diabetes. Cholesterol is another factor.
The following video shows the process of atherosclerosis and how the plaques build up inside the blood vessels, until they finally block off blood flow (resulting in a heart attack or stroke, for example).
TRADITIONAL THINKING:
For years, it has been widely accepted that “high cholesterol” is bad. We have been taught that we should keep people’s cholesterol below a certain target number in order to prevent blockages from building up in their blood vessels.
A typical discussion may have gone something like this:
Patient: “How is my cholesterol, doctor?”
Doctor: “Your bad cholesterol number is 3.5, so that is a little higher than it should be.”
Patient: “How low should it be?”
Doctor: “We should aim to keep yours less than 2.0. So I would suggest taking a cholesterol pill to get your bad cholesterol number lower.”
However, research in the last few years has shown that this may not be so simple.
RECENT RESEARCH:
In October 2015, new guidelines were published in the Canadian Family Physician journal that both simplified, yet also revolutionized, the way cholesterol is assessed and treated in primary care. A copy of the full article can be found HERE. These new guidelines are very similar to the cholesterol guideline’s in the United States that came out in 2013.
UPDATE: Canadian Family Physician (CFP) updated their cholesterol guidelines in 2024 here. Effectively, no major changes.
None suggest targeting a specific “number” for cholesterol, nor repeated testing to see what a person’s cholesterol is.
Instead of looking at cholesterol on its own, we should be looking at cholesterol in the context of an individual patient’s “overall cardiovascular risk”.
WHAT IS “CARDIOVASCULAR RISK”?
In simple terms, a person’s “cardiovascular risk” is a person’s “risk of having a heart attack or stroke in the next 10 years. There are many factors that determine a person’s cardiovascular risk, such as age, sex, smoking history, blood pressure, etc. Cholesterol levels are another factor.
Here is a video to explain how we estimate a person’s cardiovascular risk:
(The Risk Calculator shown in the video above is from Best Science Medicine).
RISK CATEGORIES:
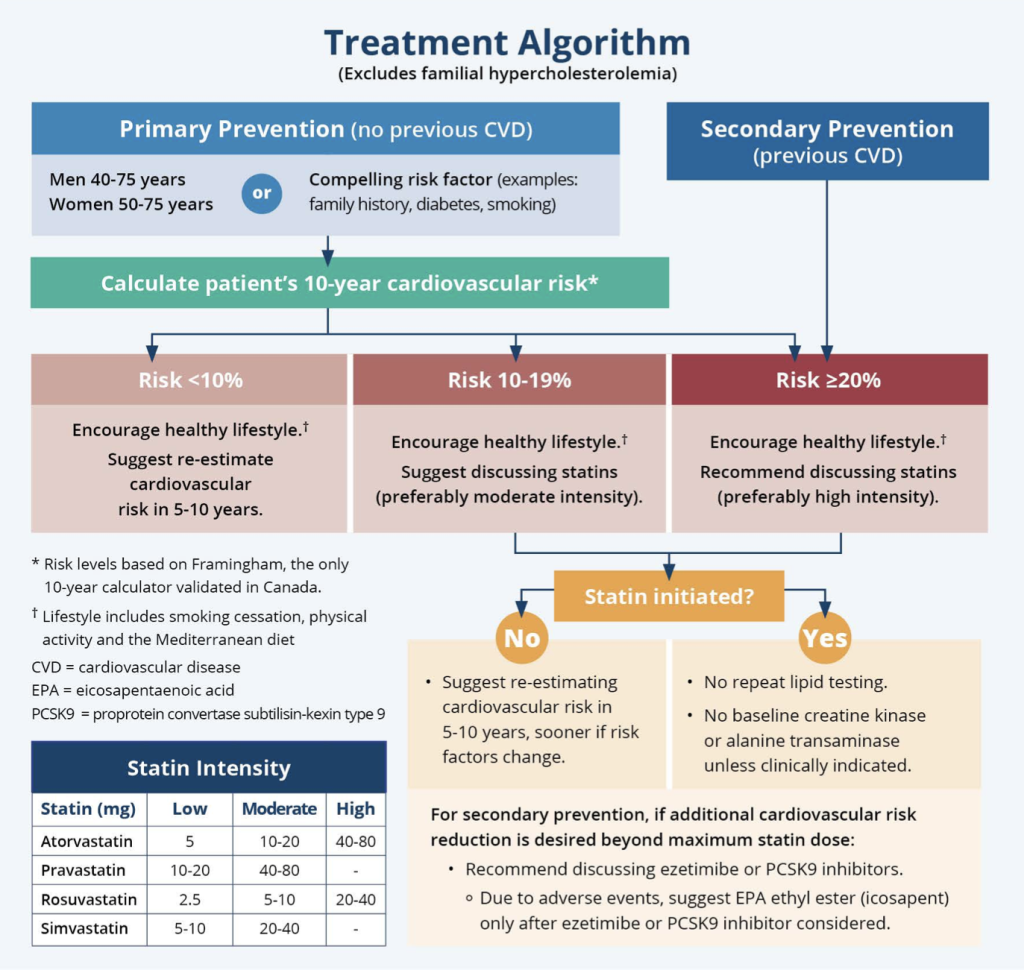
Using the calculations shown above, we can categorize a patient into “Low”, “Medium”, or “High” risk of having a heart attack or stroke in the next 10 years.
- LOW RISK = less that 10% risk
- MEDIUM RISK = between 10% to 20% risk
- HIGH RISK = more than 20% risk
Depending on the patients risk category, different prevention and treatment options may recommended.
The following is a video that compares different patients with different risk factors and how their cardiovascular risks differ. (Before watching this video, you may wish to read Dr. Stewart’s article that explains the concepts Risk Reduction).
CHOLESTEROL PILLS (“STATINS”):
When recommending ways to reduce a person’s cardiovascular risk, it is important to address ALL relevant risk factors. For example, if a person smokes, he/she should try to quit smoking. If a person has high blood pressure, he/she should try to improve it. Whether or not to be on a cholesterol pill is just one of many factors. However, this section is only going to focus on the topic of cholesterol. Furthermore, there are different types of cholesterol pills, but this section is only going to focus on the main type, called “statins“.
Research has shown that statins are the most effective type of cholesterol pill to reduce the risk of heart attacks and strokes.
KEY POINTS:
- Even though statins reduce a person’s “bad cholesterol” (LDL) levels, that may not be the actual reason they reduce a person’s cardiovascular risk.
- Studies are showing that statins seem to have an “anti-inflammatory” effect that protects our blood vessels, regardless of how high or low a person’s cholesterol level is. Even a person with traditionally “low” cholesterol may still be protected by taking a statin.
- We should think of statins as “heart protecter pills”, rather than “cholesterol pills”.
- With this in mind, a statin is recommended based on a person’s overall cardiovascular risk, rather than just the cholesterol level. (As shown above, a person’s cholesterol level is one factor that determines a person’s cardiovascular risk, but it is not the whole story).
SIMPLIFIED RECOMMENDATIONS OF FOR CHOLESTEROL PILLS
Regardless of a person’s cholesterol level, the following is recommended for heart and stroke prevention:
- LOW risk –> a statin is not recommended
- MEDIUM risk –> medium dose statin
- HIGH risk –> high dose statin
INFORMED DECISION MAKING:
Guidelines are only guidelines. There is no “correct” answer for everyone. It is up to the individual patient to know their own risks versus benefits of taking a cholesterol pill (or any other intervention, for that matter), and then make the decision that is right for him/her.
Again, before watching this video, you may wish to read Dr. Stewart’s article that explains the concepts Risk Reduction.
NO NEED TO REPEATEDLY CHECK CHOLESTEROL LEVELS:
One thing that surprises most patients about these new cholesterol guidelines is that no longer need to have their cholesterol checked every year. There are many reason for this.
As shown above, we do need a person’s initial cholesterol levels to calculate his/her overall cardiovascular risk. After that, there is rarely reason to recheck cholesterol levels more than once every 5 years.
NATURAL CHOLESTEROL LEVELS: due a genetics, everyone seems to have a “natural cholesterol level.” Some people have naturally high cholesterol; some people have naturally low cholesterol.
DIET & EXERCISE: Although diet and exercise are important, they actually have very little impact on a person’s cholesterol levels compared to their genetic predisposition. If a person decides to eat very healthily and exercise regularly, he may improve his cholesterol from 5.0 to 4.7, for example, but this will have minimal impact on the overall cardiovascular risk calculation.
LAB FLUCTUATIONS: If we take a single sample of blood and ask the lab to test that same sample two different times, we will get two different results. This is because every lab test is subject to variability and margin of error. In fact, this variability is more of a factor for cholesterol results than diet and exercise. So, when we see cholesterol levels mildly fluctuating up and down from year to year, we have no idea if this was due to lab variability or diet/exercise, for example. Again though, none of this variability has a major impact on a person’s overall cardiovascular risk estimation. Click here for a more detailed summary on lab test fluctuations.
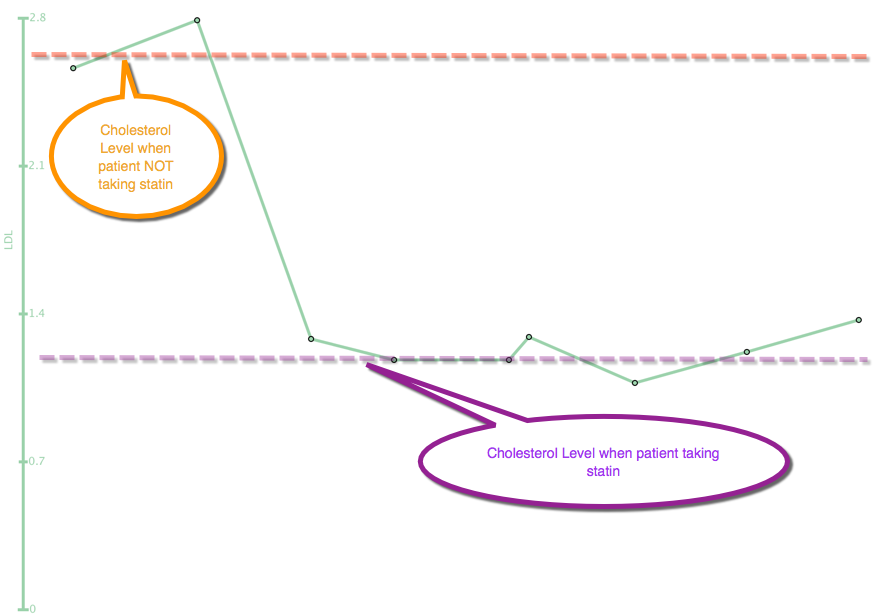
Here is a diagram that shows how little a person’s cholesterol levels vary over time, when checked repeatedly over years. The only time the cholesterol level significantly changes is when the patient is taking a statin. If the patient was to stop the statin, the cholesterol levels would bounce right back up to their natural level.
MOST IMPORTANTLY: rechecking cholesterol levels from year to year often does not change the recommendations regarding cholesterol pills. For example, if a person has a high cardiovascular risk, it would be recommended that the person should be on a high dose statin. If the person is already taking a high dose statin, the person is already on optimal treatment, so rechecking the cholesterol levels are not going to change anything!
SECONDARY PREVENTION:
All of the above discussions and examples talk about reducing a person’s risk of having a heart attack or stroke. This is known as “Primary Prevention.” That is, we want to reduce the person’s chance of having a heart attack or stroke in the first place.
But what if a person has already had a heart attack or stroke? In this case, the person is automatically deemed “High Risk.” For these patients, we are talking about “Secondary Prevention”. That is, we have to prevent having another.
Studies are very clear that for Secondary Prevention, all of these patients are “High Risk” and should be on a high dose statin.
DO STATINS CAUSE MUSCLE ACHES?
Statins have a reputation for causing muscles aches. However, this potential side effect is actually very, very rare.
Unfortunately, most patients will get muscles pains from time to time in their lives. For most people who experience muscle aches when taking a statin, most of the time is was just coincidental (meaning the muscle aches were caused by something else, rather than the statin).
In fact, a study was done where they took several patients who swore a statin was causing muscle aches. Without the patients knowing, they secretly stopped the statin pills and replaced them with “sugar pills” containing no medications. The same patients still experienced muscle pains regardless of if they were taking the real medication or the sugar pills. (The full study can be found HERE).
Please contact your primary care provider for further questions or discussions regarding your individual cardiovascular risk, and how all of this applies to you!